Often people are told that “they have Sciatica” But what does that even mean?
What does that even mean?
Sciatica is a symptom that may be originating from a plethora of pathophysiological causes.
Firstly, we should consider that the layman may understand sciatica as ANY pain that is referred into the leg, and Dr Google will often (unfortunately) confirm their suspicion of this…
When a patient presents to your clinic with a diagnosis of sciatica, it is important that we investigate much further to identify the cause of these symptoms
Where do we start?
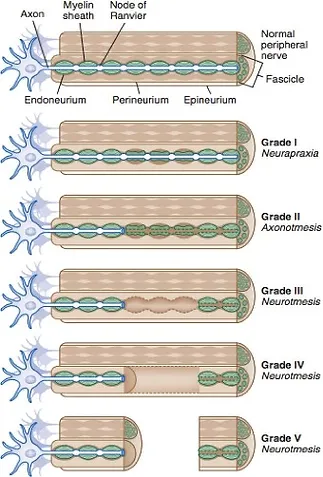
Sciatica is a symptom of compression, chemical irritation, stretch, crush injuries or even transection. This can range from focal segmental demyelination of a nerve (damage the protective connective tissue coating around the nerve), from neuropraxia, through to it being completely severed (usually from iatrogenic causes).

With the most common type of nerve injury being compression. This often occurs from bone or soft tissue compression, or external forces. (Neuropraxia as pictured above)
Nerves are very blood thirsty (you may have noticed that there is usually major nerves arteries and veins travelling together) hence these structures do not like to be compressed as this limits their oxygen, blood and impairs conductivity.
The nervous system takes in 20% of our total oxygen consumption, delivered to the nerves by small arteries called the vasa nervorum. Think of those times when you slept with your arm over your head and woke up with a dead arm. You wake up and move it around, clench your fist a few times to get some more blood flow into the area and it recovers quickly. However long-term nerve compression can have more significant implications.

If blood supply to a nerve is impaired this leads to decreased oxygen supply. This compression over an extended period can lead to fibrosis that can impair the nerve’s ability to slide in relation to surrounding tissues. These irreversible fibrotic changes can lead to demyelination and a loss of conduction of the nerve.

These chemicals include Substance P (SP) & Calcitonin Gene Related Peptide (CGRP). This can lead to a lowered nociceptor threshold leading to increased sensitivity and upregulation of the nerve activity.

Now that we understand that nerves get cranky when they are compressed, Lets have look at the anatomy of the sciatic nerve.
The sciatic nerve originates from L4-S3 nerve roots. It then passes through the greater sciatic notch beneath the piriformis through the deep gluteal space, lateral to the ischial tuberosity. Here the sciatic nerve gives rise to the muscular branch of the sciatic nerve that provides motor innervation to the hamstrings and the hamstring fibres of the adductor magnus.
The sciatic nerve continues to travel down the posterior compartment of the thigh deep to long head of the biceps femoris and superficial to adductor magnus and short head of biceps femoris.
It branches into the tibial nerve and common fibula nerve just before the popliteal fossa passing into the lower leg and further branching to provide sensory any motor innervation into the lower leg.

Why did I tell you all of this? Well, this nerve can be compressed / trapped / over stretched or irritated anywhere along its interface, which may lead to sensory or motor changes along the distribution of the nerve. So again, we need to ask more questions about their history.
1. Firstly, rule out any serious pathology including:
-
Malignancy
-
Tumor
-
Infection
-
Systemic inflammatory disorder
Do they have:
-
Pain that is increased or unrelieved with rest
-
Associated night pain, bone pain and morning stiffness
-
Visceral pain, symptoms of claudication
-
Loss of motor function
-
Bowel and bladder dysfunction
-
Saddle anesthesia
-
Fracture
-
Unexplained fever
-
Unexplained weight loss
Great now that you have taken a thorough history, we then should identify if it is a Central V’s Peripheral cause of nerve irritability / sensitivity…
Central causes of nerve irritation commonly consist of:
• Lumbosacral disc pathologies
• Lumbosacral facet syndrome
• Lumbosacral spine sprain
• Lumbosacral spondylolisthesis
• Lumbosacral spondylolysis
• Sacroiliac joint injury/dysfunction
These types of pathologies typically cause compression / irritation to the nerve root which often give rise sensory changes along a dermatomal distribution.